OSA. PAP. PSG. Being a CPAP user means you get to know a lot of confusing acronyms. Today, we’ll explore one of the most important: your AHI.
AHI stands for Apnea-Hypopnea Index, and it can tell you a lot about your sleep health, as well as the effectiveness of your CPAP therapy.
You may have encountered this term after your sleep study, or maybe as a reading on your CPAP machine, but what does it mean?
What Does AHI Mean?
Apnea-Hypopnea Index (AHI) is a measure of the severity of your sleep apnea. The calculation is a little confusing, but in simple terms it’s the average number of apneas or hypopneas you experience per hour of sleep.
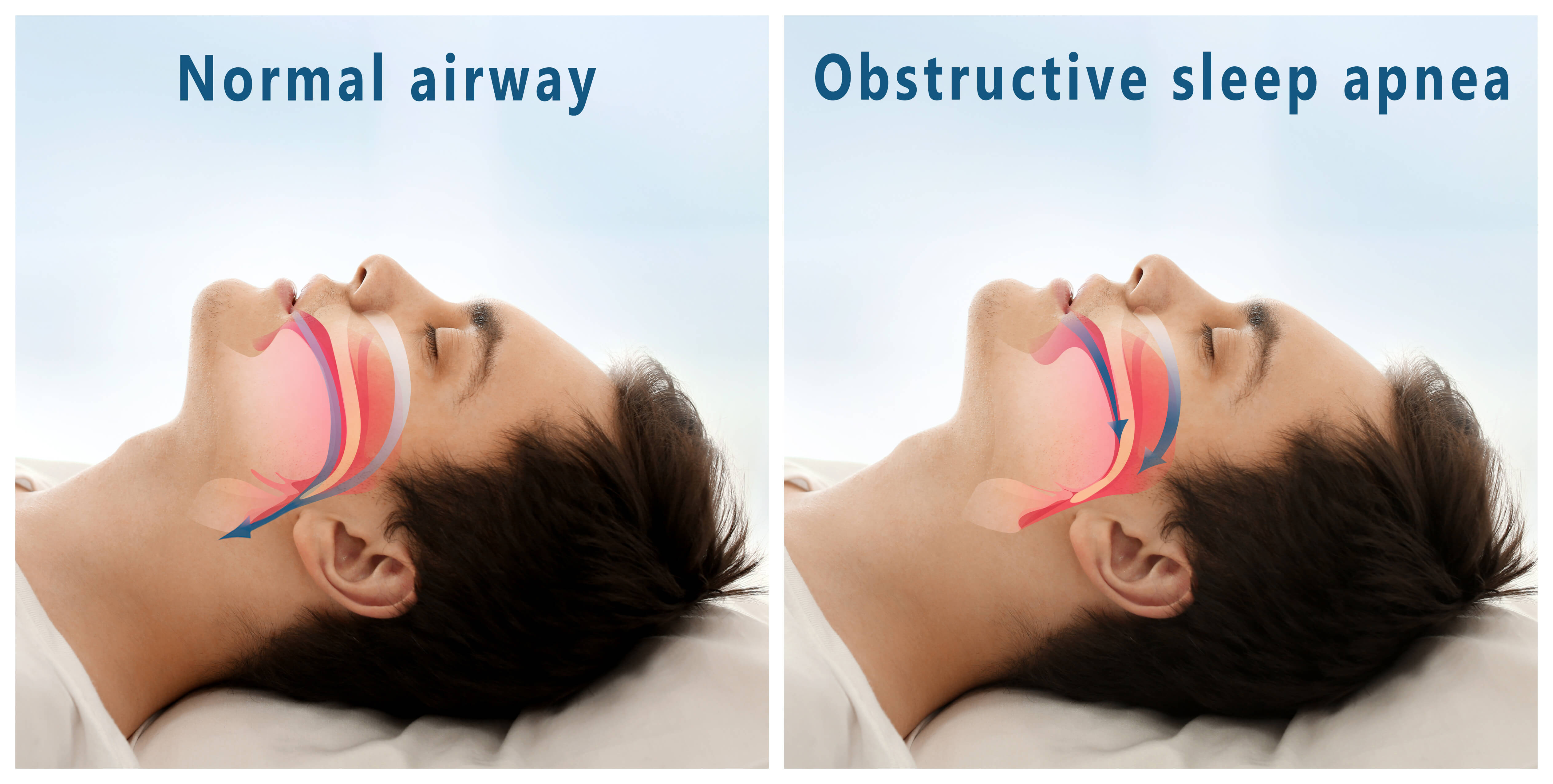
Apnea– from the Greek words for “no breath”– means a full stop in breathing for at least 10 seconds or more.
Hypopnea means a partial blockage in breathing for at least 10 seconds or more.
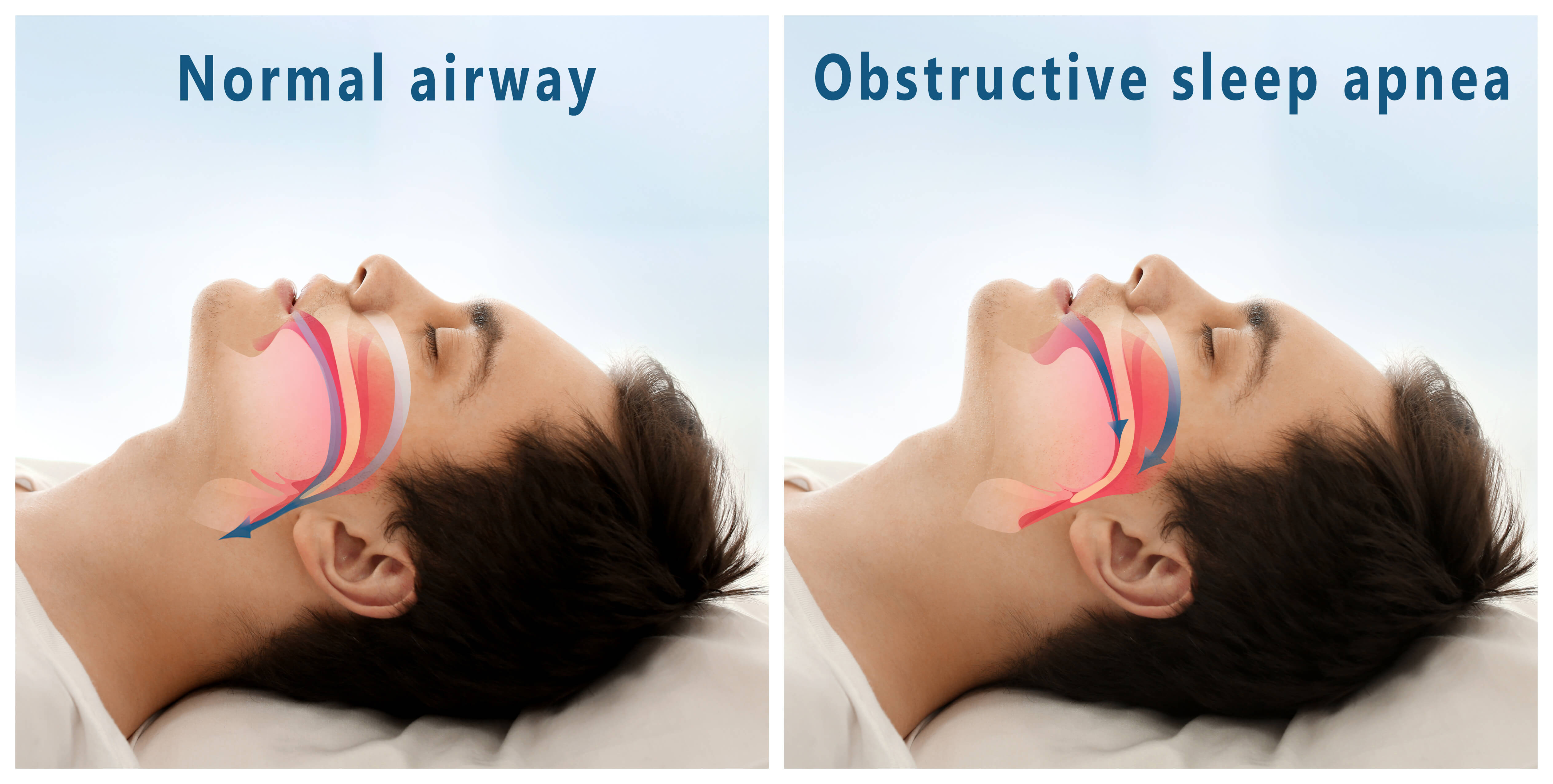
With Obstructive Sleep Apnea, these full or partial blockages occur when your soft tissues literally collapse into your upper airway and prevent airflow. So if you have, for example, an AHI of 5, that means you experience an average of 5 collapses per hour during the night.
What Is a Normal AHI?
For adults, it’s actually normal to have up to 4 apnea events per hour. An AHI under 5 is considered to show no OSA.
Let’s take a look at the AHI Scale to understand that in context...
AHI Scale
Normal - Under 5
Mild Sleep Apnea - 5-15
Moderate Sleep Apnea - 15-30
Severe Sleep Apnea - 30 or more
It’s also normal for your AHI to vary from night to night, or even throughout the night. That’s because the frequency and severity of your apneas can be affected by things like your sleeping position, mask fit, alcohol use, weight loss or gain, and other lifestyle changes.
We’ll talk about these more later, and how you can use them to lower your AHI.
What Is the Goal AHI For CPAP Treatment?
Since your AHI can change from night to night even with the use of a CPAP device, simply aiming for a specific goal AHI isn’t realistic. Instead, you should focus on reducing your average AHI over time.
While an AHI under 5 is ideal, any improvement is beneficial. Consider a person with severe sleep apnea that reduces their baseline AHI from 100 apneas per hour down to only 10. They would still qualify as having mild sleep apnea, but would also experience significant improvement in daytime sleepiness, blood pressure, and cardiovascular health!
What makes a “good” AHI for you will be determined by your doctor or sleep specialist. Your baseline AHI will be determined by a sleep study called polysomnography (PSG), and then realistic expectations for an AHI you can achieve will be based on your treatment options.
How Do I Improve My AHI Score?
CPAP pressure alone may not be enough to completely eliminate all apneas or hypopneas. And, in fact, you may see your AHI go up at times, even when you’re using your machine.
Luckily, there are some easy ways to help reduce your AHI…
1. Change your sleep position.
Sleeping on your back makes gravity work against your airways, pulling against your soft tissues, and raising your AHI. If you have positional sleep apnea, changing to a side-sleeping position will have a significant benefit!
2. Avoid alcohol before bed.
Alcohol can relax the muscles in your upper airway, making them more likely to collapse. If you see a jump in your AHI, consider skipping the nightcap.
3. Replace your mask cushion or headgear.
With regular use your cushion will wear out and your headgear will stretch, which eventually leads to mask leak. When air escapes from your CPAP mask, it means you’re not getting the proper pressure level at night.
You should replace your mask cushions every 2-4 weeks, and your headgear every 6 months.
4. Replace your CPAP mask.
Nothing lasts forever, and that includes your CPAP mask. Over time, the mask frame will stretch, bend, and warp, leading to a poor fit and a poor seal.
To prevent this before it becomes a problem, you should replace your CPAP mask every 3 months. Which is a great time to consider the next recommendation...
5. Consider a full face mask or chinstrap.
One of the most common causes of air leak is mouth leak! If you use a nasal mask, but sleep with your mouth open, you’ll lose some of your pressure out of your mouth. A full face CPAP mask or chinstrap can prevent this.
6. Have your pressure settings adjusted by your doctor or sleep specialist.
Your pressure needs can change over time, especially with changes in health status, such as significant weight loss or gain. However, adjusting your CPAP pressure should only ever be done under supervision of a healthcare professional.
If your AHI increases over time, or remains elevated, this could also be an indicator of other sleep disorders, such as central sleep apnea or complex sleep apnea. These may require alternative treatment, such as a BiPAP or auto-cpap (APAP) to ensure that your therapy can maintain the proper oxygen levels. If you notice your AHI is significantly different than normal, you should schedule a follow-up with your healthcare provider right away.